Hemodiafiltration vs Hemodialysis: A Clear Guide for Kidney Care
Kidney failure affects millions worldwide, and this guide clarifies choices between dialysis methods with clear evidence. More than 823 people per million rely on maintenance dialysis globally, underscoring dialysis demand and urgency 1. Selecting between treatment options depends on toxin load, cardiovascular risk, and long-term health goals. A thoughtful choice improves quality of life, reduces complications, and supports stability for years.
In this blog, you explore hemodiafiltration vs hemodialysis to help choose the right path for kidney care.
Key Takeaways:
- Hemodiafiltration vs Hemodialysis provides distinct benefits: Hemodiafiltration (HDF) offers better toxin removal, while HD remains more widely accessible and cost-effective.
- Hemodialysis is the preferred treatment due to its accessibility, proven outcomes, and well-established infrastructure in most healthcare settings worldwide.
- Hemodiafiltration offers enhanced removal of medium- to large-sized toxins, making it a better option for patients with cardiovascular risk and a high toxin load.
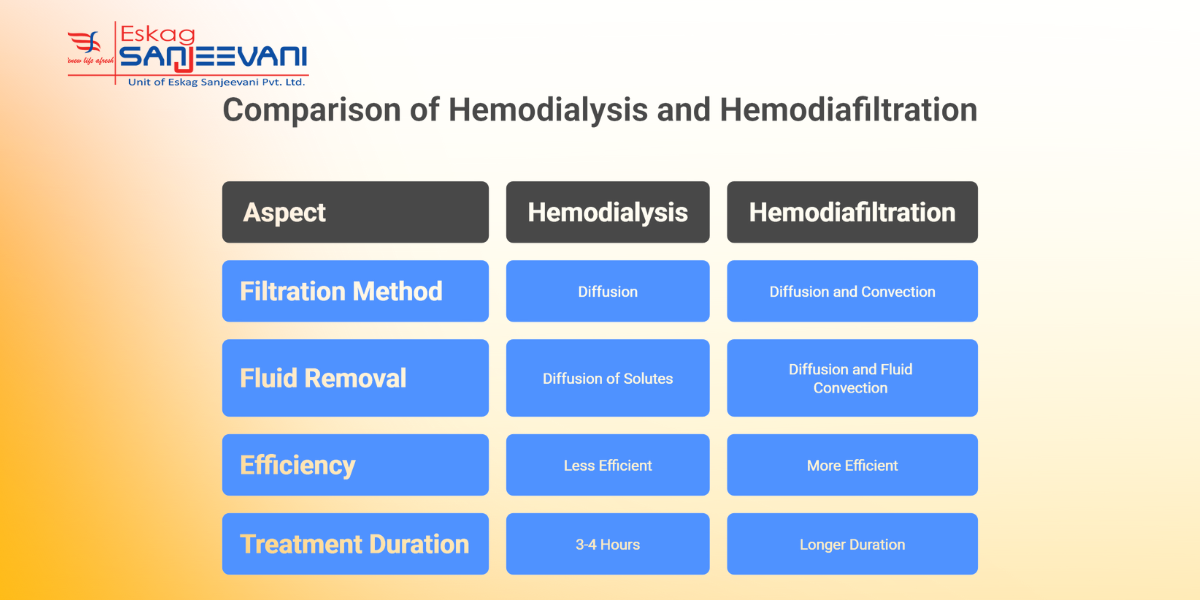
Comparing Hemodiafiltration and Hemodialysis Methods
Recent evidence suggests that patients on hemodiafiltration vs hemodialysis may experience a roughly 23% lower all‑cause mortality compared with standard hemodialysis (HD), under optimal conditions 2. Still, the choice between hemodiafiltration vs hemodialysis depends heavily on patient condition, vascular access quality, and treatment resources.
A realistic comparison of both modalities helps patients and doctors decide what fits each case best.
- Toxin Clearance Profile: HDF combines diffusion and convection, enhancing the removal of medium to large “middle‑molecule” toxins that HD alone may miss. In contrast, HD relies mainly on diffusion, which clears smaller solutes like urea efficiently, but may leave larger toxins behind.
- Mortality and Cardiovascular Outcomes: Meta‑analysis shows that HDF is associated with lower all‑cause and cardiovascular mortality compared with HD, with a risk ratio of 0.81 for overall mortality 3. That said, some trials find no significant difference, so the benefit may depend on achieving high convection volumes and maintaining clean dialysate.
- Fluid and Salt Removal Precision: HD offers predictable, well‑established fluid removal schedules, making it easier to manage ultrafiltration and blood‑pressure stability session to session. HDF’s convection component can aid the removal of fluid and toxins together, but demands precise vascular access and monitoring, which may not suit all patients.
- Resource, Cost, and Practical Considerations: HD remains widely available and simpler to deliver worldwide due to lower technical demand. HDF requires high-quality water treatment systems, skilled staff, and stable vascular access, factors that raise cost and limit universal availability.
- Patient Suitability and Flexibility: HD is suitable for a broad range of patients, including those with fragile vascular access, older age, or limited treatment centre infrastructure. HDF may benefit patients with high toxin burden, cardiovascular risk, or need for enhanced clearance, but only if infrastructure and patient factors align properly.
Here are some of the clinical benefits of kidney dialysis, hemodialysis and haemodiafiltration for a better understanding of kidney dialysis.
Clinical Benefits of Hemodialysis and Haemodiafiltration
Hemodiafiltration vs hemodialysis offers distinct clinical benefits based on patient condition, procedure requirements, and treatment goals, with each method excelling in certain areas.
Here are some of the benefits of Hemodialysis and haemodiafiltration:
- Removal of Small Toxins: Hemodialysis effectively clears small toxins such as urea and creatinine, providing consistent, reliable results, especially for those with early-stage kidney failure.
- Superior Middle Molecule Clearance: Hemodiafiltration excels at removing larger uremic toxins, including β2-microglobulin, which reduces the risk of long-term complications such as amyloidosis and bone disease.
- Wider Availability and Simplicity: Hemodialysis is easier to implement across diverse healthcare settings, from hospitals to resource-limited areas, making it a widely accessible treatment option.
- Improved Long-Term Outcomes: Hemodiafiltration has been shown to reduce inflammation and improve cardiovascular health, potentially lowering the risk of cardiovascular disease in long-term dialysis patients.
Let’s now explore the basics of hemodialysis and why it is a preferred option among individuals.
Hemodialysis: Why It’s Still the Preferred Treatment Option
Hemodialysis remains the preferred treatment for kidney failure due to its proven efficacy in removing toxins and managing fluid volume. It is widely accessible, with established protocols in both high- and low-resource settings, enabling it to reach a broad patient population. The procedure is well understood by healthcare professionals, ensuring that patients receive consistent, reliable care.
Hemodialysis offers the flexibility of frequent treatment schedules, allowing patients to adjust their sessions to fit personal and lifestyle needs. Despite the rise of alternative methods such as haemodiafiltration, hemodialysis remains the gold standard due to its affordability and long clinical track record.
To better understand the process, let’s explore how hemodiafiltration dialysis works in detail.
Understanding the Hemodiafiltration Procedure and Process
Hemodiafiltration combines two processes: diffusion, which removes small toxins, and convection, which helps eliminate larger waste molecules. The procedure uses a semi-permeable membrane through which blood passes, allowing waste products to be removed from the blood into the dialysate.
A key part of HDF is the substitution fluid, which helps replenish plasma volume and ensures efficient toxin removal during the process. The process requires a higher volume of blood flow and dialysate compared to traditional hemodialysis to achieve optimal clearance. Hemodiafiltration is typically more complex, requiring precise monitoring of fluid balance and convection rates to ensure patient safety and optimal outcomes.
When deciding hemodiafiltration vs hemodialysis, consider patient needs, treatment goals, and resources.
Hemodiafiltration vs Hemodialysis: Choosing the Right Option
The choice for hemodiafiltration and hemodialysis depends on patient needs, the severity of kidney failure, and treatment goals. While modalities manage waste clearance, hemodiafiltration may offer enhanced removal of medium-sized toxins.
Hemodialysis, however, remains the more commonly used approach due to its simplicity, widespread availability, and well-established protocols in clinical practice.
- Vascular Access and Treatment Time Requirements: Hemodialysis requires an arteriovenous fistula or graft, which can be easier to establish in patients with suitable veins. Hemodiafiltration often demands higher blood flow rates and a more complex setup, making temporary catheter access less effective in ensuring optimal clearance.
- Inflammation and Cardiovascular Protection: Studies indicate that hemodiafiltration vs hemodialysis can reduce inflammation markers, such as C-reactive protein (CRP), and improve cardiovascular outcomes. For patients with high cardiovascular risk, HDF may help minimise the systemic inflammation that contributes to cardiovascular morbidity in end-stage kidney disease.
- Long-Term Impact on Uremic Toxin Removal: Hemodiafiltration provides clearance of uremic toxins with chronic kidney disease (CKD), such as phosphate and parathyroid hormone.
- Resource and Infrastructure Requirements: Hemodialysis remains more accessible due to its simpler infrastructure and lower maintenance requirements. Hemodiafiltration, however, requires more advanced dialysis machines, water treatment systems, and skilled staff to manage the increased complexity of the procedure.
Also read: Types of Dialysis: Exploring Options for Kidney Failure Treatment.
How Eskag Sanjeevani Dialysis Can Assist You With Hemodialysis
Selecting the best dialysis treatment, whether hemodiafiltration vs hemodialysis, depends on your health needs, resources, and treatment goals. It’s essential to work with healthcare teams to determine the options on factors like toxin clearance, cardiovascular health, and kidney function. Early decision-making can significantly improve long-term outcomes.
Eskag Sanjeevani Dialysis provides comprehensive care with a well-established dialysis unit, offering both hemodialysis and specialised care for patients with complex needs. Whether you require hemodialysis for consistent care or are exploring other treatment options, Eskag Sanjeevani ensures you receive optimal support. Their skilled staff and high-quality equipment in dialysis centres are tailored to each patient’s long-term kidney health needs.
Hemofiltration (HDF) uses both diffusion and convection to remove toxins, allowing the clearance of larger molecules. In contrast, hemodialysis relies on diffusion for toxin removal, typically targeting smaller solutes like urea and creatinine
HDF requires more complex equipment, higher blood flow rates, and a specialised setup, which makes it less widely available. Additionally, the procedure tends to be more expensive than conventional hemodialysis due to increased monitoring requirements and resource needs.
Dialysis does not restore kidney function; it only temporarily replaces the filtration function. However, in cases of acute kidney failure, the kidneys may recover over time if the underlying cause is treated; this is less common in chronic kidney failure.
Hemodialysis is generally not recommended if a patient has severe cardiovascular instability or a poor vascular access site. Additionally, it is unsuitable for patients who are unwilling to commit to long-term treatment and those with life-limiting conditions without clear potential for recovery.
The primary alternative to dialysis is a kidney transplant, where a healthy kidney from a donor is surgically placed into the recipient. Other non-dialysis options may include conservative management, focusing on symptom control and quality of life in patients who cannot undergo dialysis or transplantation.