AV Fistula Not Working? 3 Signs of Blockage You Can't Ignore
If you depend on dialysis, your AV fistula is more than a surgical connection; it is your lifeline. When you notice a sign of blockage, even a subtle change can create anxiety and uncertainty. Many patients struggle to decide whether a symptom is minor or a serious warning that needs urgent care. Early recognition and timely medical review can often save access and prevent emergency catheter placement. In this blog, you will learn how to identify warning signs, understand causes, and take prompt action to protect your fistula.
In this blog, you will learn how to identify warning signs of blockage, understand causes, and take timely action to protect your fistula.
Key Takeaways:
- Loss of thrill or bruit is often the earliest warning of AV fistula blockage.
- Arm swelling, colour change, or dialysis flow issues require urgent medical evaluation.
- Early intervention improves fistula survival and reduces the cost of repeat procedures.
Quick Answer: The most critical signs of AV fistula blockage include loss of vibration, arm swelling or colour change, and dialysis machine flow problems.
Quick Links
What is an AV Fistula and Why Does it Get Blocked?
An AV fistula is a surgical join between an artery and a vein that creates high-flow access for haemodialysis. If you notice any signs of blockage, it often points to reduced flow due to narrowing or clotting and requires prompt review.
- What it does: Higher blood flow through the vein makes repeated dialysis needle access safer than many alternatives.
- Why “blockage” happens: Peripheral vein stenosis (narrowing) is a primary driver of fistula and graft thrombosis.
- Where narrowing often sits: In fistulas, stenosis commonly occurs near the anastomosis or the outflow vein, between 70% and 85%, leading to poor flow 1.
- How the narrowing forms: Vessel injury plus smooth-muscle growth (neointimal hyperplasia) can follow turbulent flow, needle trauma, or repeat procedures.
- Why it matters for dialysis quality: When access flow drops, dialysis can become inefficient, leading to cannulation difficulty or prolonged bleeding post-dialysis.
- A practical technical benchmark: The “Rule of 6s” uses targets such as ≥600 mL/min flow and ≥6 mm vein diameter as common maturation checks 2.
Next, let’s explore the key signs of AV fistula blockages that can make dialysis sessions difficult.
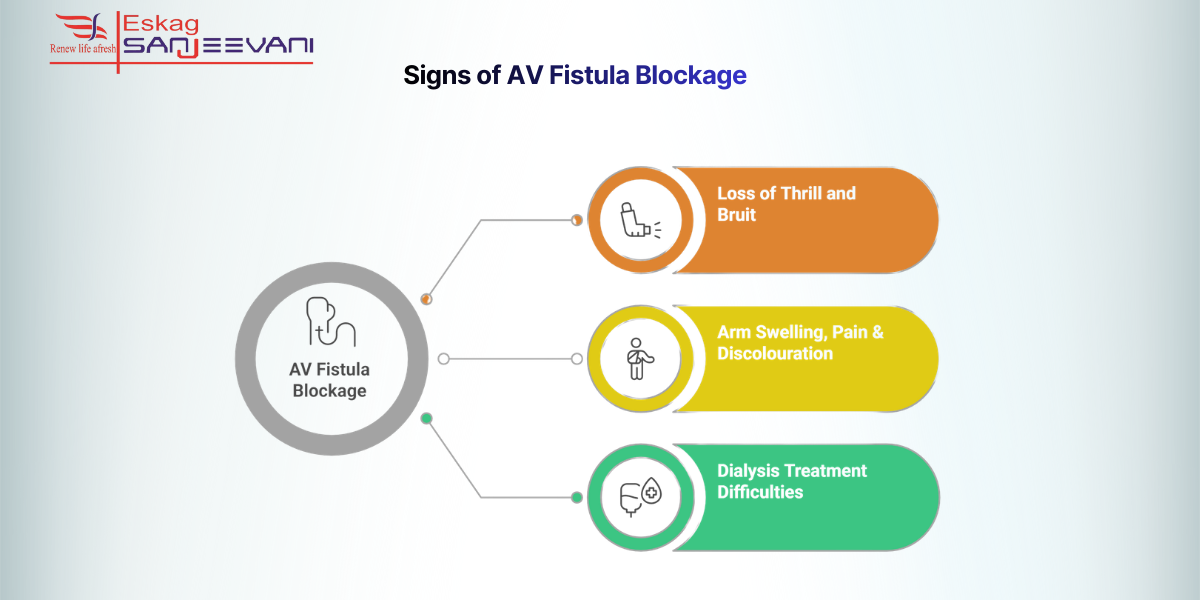
3 Signs of AV Fistula Blockage
If you notice any signs of blockage in your access arm, early recognition can help protect your AV fistula for dialysis and prevent complete clotting.
1. Loss of Thrill and Bruit
A healthy AV fistula for dialysis produces a constant buzzing vibration, called a thrill, and a whooshing sound, called a bruit, both reflecting steady blood flow. If the thrill weakens, becomes intermittent, or disappears, it may indicate reduced flow from stenosis or thrombosis, which are leading causes of access failure. Clinical guidance suggests that sudden loss of thrill often signals acute clotting and requires urgent vascular evaluation.
2. Arm Swelling, Pain & Discolouration
Swelling of the fistula arm, new pain, tightness, or colour change (pale, bluish, or dusky tone) may reflect impaired venous outflow or clot formation. Venous hypertension or central vein stenosis can cause visible vein enlargement and persistent arm oedema, as described in the vascular access literature. Severe pain, cold fingers, or numbness can also indicate steal syndrome, which needs urgent specialist assessment.
3. Dialysis Treatment Difficulties
Dialysis machine alarms for low blood flow or rising venous pressure often signal internal narrowing before complete failure occurs. Studies in peer-reviewed journals explain that reduced access flow increases recirculation and compromises dialysis adequacy, sometimes reflected in low Kt/V values.
A Kt/V of <1.2, or an interval decrease by more than 0.20, should prompt intervention to increase dialysis adequacy and forestall potential access thrombosis 3. Prolonged bleeding after needle removal or repeated cannulation difficulty may also reflect stenosis, reinforcing the medical definition of blockage, meaning restricted blood passage within the fistula circuit.
With a better understanding of the signs of blockage, let’s explore the primary causes and potential risks associated with AV fistula.
Causes of AV Fistula Blockage and Risk Factors You Should Know
AV fistula blockage does not happen suddenly in most cases; it usually develops from progressive vessel changes after the AV fistula procedure. If you live with chronic kidney disease and depend on long-term dialysis access, understanding these mechanisms helps you prevent avoidable failure.
- Stenosis (vessel narrowing): Neointimal hyperplasia is the most common cause of AV fistula dysfunction and precedes most thrombosis events; one review reports stenosis in up to 78% of failing accesses 4.
- Thrombosis (clot formation): Thrombosis often occurs on top of untreated stenosis and may completely block blood flow; reported AV fistula thrombosis rates range from 0.1 to 0.5 episodes per patient-year 5.
- Venous hypertension and central vein stenosis: Prior central venous catheters can damage central veins, causing backpressure, arm swelling, and reduced outflow from the fistula
- Intradialytic hypotension: Repeated low blood pressure episodes during dialysis reduce access flow, increasing clot risk and compromising fistula patency.
- Infection and inflammation: Perivascular infection and chronic inflammatory states seen in end-stage kidney disease contribute to endothelial injury and a prothrombotic tendency.
- Mechanical stress and dehydration: Compression from tight clothing, trauma to the fistula arm, or excessive fluid removal between sessions may reduce flow and predispose to access failure.
Also read: Kidney Failure Treatments: A Complete Patient Guide.
What to Do When Your AV Fistula is Blocked: Treatment Options
An AV fistula blockage is a medical urgency because delayed action can lead to complete access failure and missed dialysis sessions. Early reporting and timely vascular intervention often restore flow and prevent the need for a new access site.
Here’s what you should do immediately if you have a blocked AV fistula:
- Contact your dialysis team immediately if you notice a loss of thrill, swelling, or poor machine flow; do not wait until your next session.
- Undergo prompt diagnostic evaluation, usually a Doppler ultrasound to assess blood flow and identify stenosis or clot location; angiography confirms severity.
- Avoid compressing the fistula arm, including blood pressure cuffs, tight clothing, heavy lifting, or sleeping on that side.
- Maintain adequate hydration between sessions (as advised by your nephrologist) to preserve blood flow and reduce the risk of clots.
- Perform daily thrill checks and report any changes immediately to improve the chances of a successful salvage.
- Wear medical alert identification indicating dialysis access to prevent accidental procedures on the fistula arm in emergencies.
Here are some of the treatment options for a blocked AV fistula:
| Treatment Option | What It Involves | When It Is Used |
| Thrombectomy | Catheter-based clot removal using mechanical devices or clot-dissolving medication (e.g., tPA) | Acute thrombosis with recent clot formation |
| Angioplasty | Balloon inflation inside the narrowed segment to restore blood flow | Stenosis identified on imaging; often combined with thrombectomy |
| Stent Placement | A mesh tube is inserted to keep the vessel open if the narrowing recurs | Recurrent stenosis or elastic recoil after angioplasty |
| Surgical Revision | Open surgery to repair or recreate access | Repeated failure, large clot burden, or complex anatomy |
Reported technical success rates for endovascular thrombectomy range between 70-90% when treated early 6.
Cost Considerations in India
In India, early thrombectomy may cost approximately ₹25,000-₹50,000, depending on the hospital and city. In comparison, AV fistula for dialysis costs in India for creating a new access can range from ₹50,000 to ₹1.5 lakh or more in private settings.
Preventive monitoring at experienced dialysis centres, including structured surveillance and vascular review, reduces complication rates and repeat procedures.
Final Thoughts
Your dialysis access deserves daily attention because small changes can signal larger problems. If you notice reduced vibration, swelling, or prolonged bleeding, inform your care team immediately. Early treatment often restores blood flow and prevents the need for a new AV fistula procedure. Keep regular follow-ups, follow arm-care precautions, and never ignore persistent symptoms. Centres experienced in vascular access care, including Eskag Sanjeevani, emphasise early reporting and structured monitoring to improve long-term fistula survival.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5332078/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9374077/
- https://cdt.amegroups.org/article/view/16884/html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5332078/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5778528/
- https://evtoday.com/articles/2023-june/tips-tricks-and-pitfalls-for-thrombosed-avfs
Medical Disclaimer: This content is for educational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult your nephrologist or vascular specialist for personalised guidance regarding your AV fistula.
A healthy AV fistula usually provides blood flow above 600 mL/min for effective dialysis. Machines target pump speeds around 300–500 mL/min. Persistent low flow suggests possible stenosis.
Repeated intradialytic hypotension reduces access perfusion. Reduced flow promotes clot formation within narrowed segments. Careful fluid removal protects fistula patency.
Yes, diabetes accelerates vascular damage. Poor glycaemic control promotes inflammation and endothelial dysfunction. Strict sugar control improves long-term access to survival.
Well-maintained fistulas can function for 5–10 years or longer. Longevity depends on vessel quality and monitoring. Early intervention prevents premature failure.
Recirculation mixes cleaned blood with untreated blood. This lowers urea clearance efficiency. Persistent recirculation requires access evaluation.