Is Home Dialysis Right for You? Comparing Costs and Comfort
Kidney failure changes daily life in ways that feel overwhelming at first. You may wonder whether frequent hospital visits are your only option. Home dialysis offers an alternative that combines medical treatment with greater flexibility. Yet comfort, cost, safety, and long-term support all matter before you decide.
In this blog, you will understand whether home dialysis suits your health, lifestyle, and financial planning in India.
Key Takeaways:
- Home dialysis offers flexibility but requires strict adherence to hygiene protocols, training, and regular nephrologist supervision.
- Costs vary widely in India, influenced by therapy type, city, consumables, and monitoring needs.
- Strong centre backup improves safety, especially during emergencies or complications at home.
Quick answer: Home dialysis is possible for selected patients, but centre-based dialysis remains the safest and most structured option for many, especially when regular supervision and immediate medical support are priorities.
Quick Links
- What Is Home Dialysis?
- Is Home Dialysis Possible in India?
- 2 Types of Home Dialysis: PD vs Home Haemodialysis
- Who Can Do Home Dialysis? Eligibility Criteria
- Home vs Centre Dialysis: Comfort and Lifestyle
- Cost of Home Dialysis in India
- Government Support & Financial Schemes
- Risks and Complications of Home Dialysis (Must Read)
- Why Centre Support Still Matters
What Is Home Dialysis?
Home dialysis is a form of treatment for kidney failure that lets a dialysis patient receive regular kidney replacement therapy at home with clinical oversight. Instead of travelling to a centre for sessions, you or a caregiver performs the therapy in a familiar environment, following a schedule set by your nephrologist.
Here are some of the key elements for home dialysis
- Treatment at home: Home dialysis can be done in your own space rather than a hospital or dialysis unit.
- Two main types: Peritoneal Dialysis (PD) and Home Haemodialysis (HHD).
- Clinical oversight: You remain under a nephrologist’s care, with regular monitoring and training before starting.
- Flexible schedule: Many patients can fit treatments around daily routines.
- Care partner support: For HHD, a trained helper may be needed initially.
Is Home Dialysis Possible in India?
Yes, home dialysis can be done in India, but its adoption remains limited compared with in-centre treatment. The basic principle is the same as in centre care: a dialysis patient performs prescribed therapy in a home setting under the oversight of a nephrologist and a trained care team.
According to PMC, about 11% of all dialysis patients worldwide receive peritoneal dialysis (a home modality), and the use of home modalities such as home haemodialysis is even lower in many regions 1.
- Home dialysis works in India: You can receive kidney failure therapy at home through either PD or home haemodialysis.
- Clinical suitability: Not every kidney failure patient can perform dialysis at home. A nephrologist assesses medical factors, home conditions, and support systems before recommending it.
- Medical stability: Hemodynamically stable patients without severe heart disease or uncontrolled diabetes
Home infrastructure: Clean, dedicated space with reliable electricity and water supply - Cognitive ability: Capacity to learn and follow complex procedures
Manual dexterity: Ability to handle equipment and perform sterile techniques - Support system: Availability of a trained care partner for emergencies
- Medical stability: Hemodynamically stable patients without severe heart disease or uncontrolled diabetes
Contraindications (who cannot do home dialysis): Severe visual impairment preventing sterile technique. Advanced dementia or severe cognitive impairment. Unstable cardiovascular disease. Patients with active abdominal infections or recent abdominal surgery.
- Training requirement: Before starting home dialysis, you and a caregiver complete structured training (often several sessions) with your dialysis team to learn procedures, safety protocols, hygiene practices, and emergency procedures.
- Care partner role: Many patients need a trained care partner at home to help with setup and treatment steps, especially for home haemodialysis.
Next, let’s understand the two primary approaches to home dialysis.
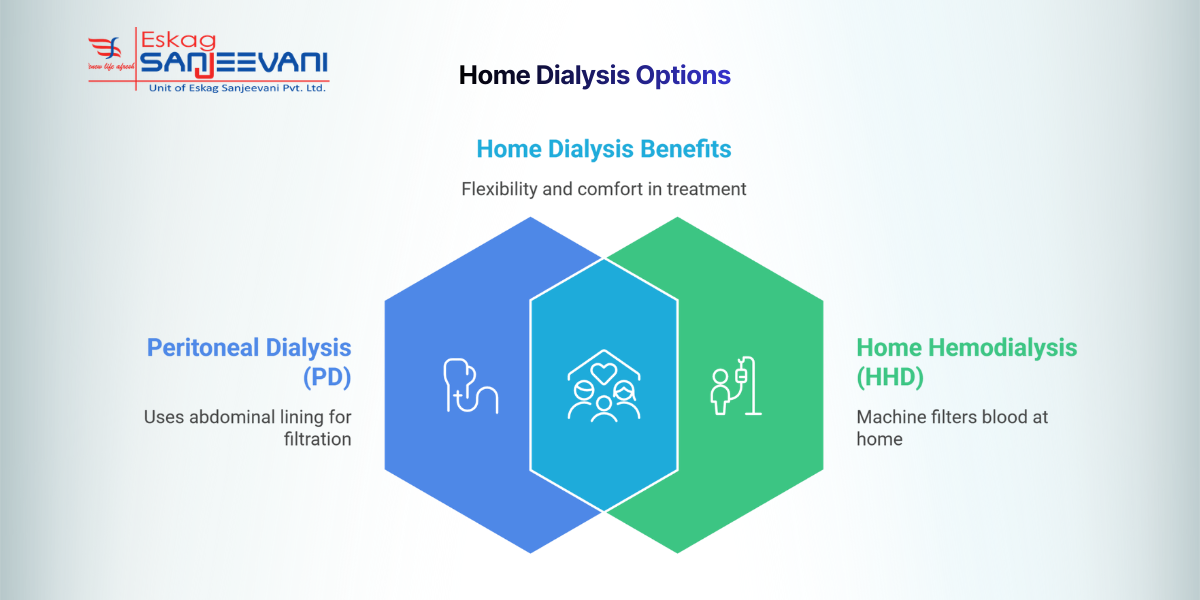
2 Types of Home Dialysis: PD vs Home Haemodialysis
Dialysis at home can be performed through two main approaches: Peritoneal Dialysis (PD) and Home Haemodialysis (HHD), each with distinct processes, schedules, and suitability depending on medical and home factors.
1. Peritoneal Dialysis (PD)
Peritoneal Dialysis uses the lining of your abdomen, called the peritoneum, as a natural filter to remove waste and excess fluid. A sterile dialysis solution flows into the abdominal cavity through a soft catheter, stays for a few hours, and then drains out with toxins. In India, approximately 8-17% of the total population is affected by chronic kidney diseases (CKD), showcasing that PD is an underutilised method despite being a home-based option 2.
Two PD methods:
- CAPD (Continuous Ambulatory Peritoneal Dialysis): Manual exchanges 3-4 times daily, each taking 30-40 minutes.
- APD (Automated Peritoneal Dialysis): A machine performs exchanges overnight while you sleep, typically for 8-10 hours.
2. Home Haemodialysis (HHD)
Home haemodialysis uses a compact dialysis machine installed at home to clean the blood through a dialyser, similar to in-centre haemodialysis. Blood flows through a vascular access, such as an arteriovenous fistula, and returns to the body after filtration. A dialysis patient usually requires structured training and often a care partner to manage machine setup, needle placement, and alarms safely.
Here is a tabular representation for peritoneal and haemodialysis:
|
Feature |
Peritoneal Dialysis (PD) |
Home Haemodialysis (HHD) |
|
How it works |
Uses the abdominal lining as a filter |
Uses a machine and an artificial dialyser |
|
Access type |
Abdominal catheter |
Fistula or graft |
|
Frequency |
Daily exchanges (CAPD/APD) |
Usually 3–6 sessions per week |
|
Equipment need |
Dialysis fluid and basic supplies |
Dialysis machine and water setup |
|
Care partner |
Often not mandatory |
Often required |
|
Travel flexibility |
Easier to travel with supplies |
More equipment-dependent |
Note: Both approaches allow dialysis at home with clinical oversight. The right choice depends on medical condition, home readiness, lifestyle, and your nephrologist’s assessment.
Who Can Do Home Dialysis? Eligibility Criteria
Not every dialysis patient is a suitable candidate for home-based treatment. Your nephrologist will evaluate multiple factors before recommending home dialysis:
- Medical eligibility: Hemodynamically stable (stable blood pressure, no severe heart failure). Patients with no severe uncontrolled diabetes with complications
- Patient capabilities: Mental capacity to learn and remember complex procedures, with good vision or corrected vision for sterile technique. Patients with manual dexterity to handle equipment.
- Home requirements: Clean, dedicated space for dialysis (minimum 10×10 feet). Reliable electricity supply (with backup for HD). Clean water source (RO plant for HD; potable water for PD storage). Proper storage space for supplies (dry, temperature-controlled)
- Support system: Available family member or caregiver for training. Backup support for emergencies. Access to transport for centre visits.
If you don’t meet these criteria, centre-based dialysis remains the safer and more appropriate option for your treatment.
Home vs Centre Dialysis: Comfort and Lifestyle
Choosing between home dialysis and centre-based dialysis affects your daily routine, independence, and overall comfort as a dialysis patient, and the right option depends on how well the treatment fits your medical needs and lifestyle.
Here is a tabular representation to understand the difference between the prospects of home dialysis and centre-based dialysis:
| Feature | Home Dialysis | Centre-Based Dialysis |
| Time Commitment | The treatment schedule can be adjusted within the prescribed plan. PD is often daily, while home haemodialysis may vary in frequency. | Usually done 3 times per week, with each session lasting about 4 hours, excluding travel time. |
| Travel Burden | No routine travel required once training is complete. | Regular travel to and from the dialysis centre is required. |
| Flexibility | Greater control over timing; night-time or personalised schedules may be possible. | Fixed appointment slots based on centre availability. |
| Comfort & Environment | A familiar home setting may reduce stress and improve convenience. | Supervised clinical setting with immediate access to trained staff. |
| Medical Support | Requires training, hygiene discipline, and scheduled reviews with the nephrology team. | Continuous professional supervision during every session |
| Lifestyle Impact | May allow better work continuity and family time if well managed. | Structured routine may offer reassurance but can limit schedule flexibility. |
| Quality control | Dependent on patient adherence to protocols. | Professional quality assurance every session. |
The decision should balance medical safety, personal comfort, caregiver availability, and long-term sustainability under nephrologist supervision.
Also read: SLED Dialysis: A Hybrid Approach to Kidney Failure Treatment.
Cost of Home Dialysis in India
Dialysis in India involves ongoing medical and financial commitments, and total costs vary depending on therapy type, city, facility category, and eligibility for government support. Since dialysis is long-term care rather than a one-time treatment, financial sustainability matters as much as clinical suitability.
Here is a tabular representation of the estimated dialysis costs in India in 2026:
|
Category |
In-Centre Haemodialysis |
Home Peritoneal Dialysis (PD) |
Home Haemodialysis (HHD) |
|
Per Session Cost |
₹750–3,000 (private), ₹150-1,500 (Govt. centres) |
Not per session (daily exchanges) |
₹2,000–3,500 (consumables only) |
|
Monthly Cost |
₹9,000–36,000 (12 sessions) |
₹20,000–30,000 (consumables, varies by model) |
₹24,000–42,000 (12 sessions, excl. setup) |
|
One-Time Setup |
None |
Catheter: ₹15,000–40,000 |
Equipment + setup: ₹5–8 lakh |
|
Annual Estimate |
₹1.08–4.32 lakh |
₹2.4–3.6 lakh (approx., varies widely) |
₹2.88–5.04 lakh (excl. depreciation) |
Note: Actual costs depend on prescription frequency, city, hospital category, and insurance eligibility.
Here are some of the core factors that affect overall cost:
- Type of therapy: PD involves daily consumables; HHD requires high initial equipment investment.
- Government vs private setting: Public and PPP centres significantly reduce per-session costs.
- City variation: Metro private centres typically cost more than district facilities.
- Additional medical expenses: Erythropoietin, iron therapy, phosphate binders, and lab tests may cost ₹7,000–20,000 per month.
- Insurance & subsidies: Coverage dramatically changes out-of-pocket burden.
Without subsidy or insurance, long-term dialysis can be financially challenging for most Indian families.
Government Support & Financial Schemes
Here are some government support schemes available in India for dialysis patients.
1. Pradhan Mantri National Dialysis Programme (PMNDP)
PMNDP operates under the National Health Mission and provides free haemodialysis services at district hospitals and PPP centres. The programme covers all states and union territories, significantly expanding access for economically vulnerable patients. Peritoneal dialysis support is available in selected locations, though coverage varies by centre.
2. Ayushman Bharat (PM-JAY)
PM-JAY provides health coverage of up to ₹5 lakhs per family per year to eligible households. Dialysis, including related hospitalisation and medication support, is covered at empanelled hospitals. Eligibility depends on socioeconomic criteria.
Now, let’s explore some of the risks that are common during home dialysis sessions.
Risks and Complications of Home Dialysis (Must Read)
Home dialysis can offer flexibility, but it carries real medical risks that require careful training, monitoring, and ongoing clinical support to manage safely.
- Infections (PD and HHD): Peritoneal dialysis is associated with peritonitis, with international data showing rates of 0.3–0.6 episodes per patient-year in well-performing programs 3. Exit-site infections are also common and can lead to catheter removal.
- Vascular Access Complications (HHD): Arteriovenous fistulas and grafts can clot, narrow, or become infected. Access dysfunction remains one of the leading causes of hospitalisation among haemodialysis patients.
- Cardiovascular Instability: Blood pressure fluctuations during dialysis are common. Intradialytic hypotension occurs in approximately 15–30% of haemodialysis sessions globally 4.
- Technique Failure & Transition: Over time, some PD patients may need to switch modalities due to membrane changes or recurrent infections. Technique survival varies by centre but declines over the years of therapy.
- Emergency & Training Challenges: Home therapy requires early recognition of complications. Delayed emergency response, incomplete training, or caregiver fatigue can increase risk and lead some patients to return to centre-based care.
Also read: Top 10 Dialysis Side Effects and When to Seek Medical Help.
Why Centre Support Still Matters
Even when dialysis at home is an option, ongoing support from established dialysis centres remains essential for safety, expert guidance, and continuity of care.
- Access to expert care: Eskag Sanjeevani’s network of over 170 dialysis centres provides trained nephrology teams and modern equipment, so patients have reliable clinical support whenever needed — whether for initial training or complex medical review.
- Emergency readiness and monitoring: Regular follow-ups and emergency backup at established dialysis centres ensure prompt intervention if complications arise during home treatment, offering peace of mind alongside the convenience of home treatment.
- Dialysis near me support: With so many centres across India, patients can easily locate “dialysis near me”, helping them access supervised sessions, lab monitoring, and crisis-ready care even if they travel or return to centre-based therapy.
Final Thoughts
Choosing between home and centre treatment is not only about convenience; it is about long-term safety and sustainability. You should discuss clinical suitability, infection risks, caregiver availability, and financial planning with your nephrologist before making a decision. A dialysis patient benefits most from structured follow-ups, regular lab monitoring, and clear emergency pathways.
If you consider home therapy, ensure that a reliable network of dialysis services remains accessible nearby. Dialysis centres of Eskag Sanjeevani provide ongoing oversight and emergency backup, helping you balance independence with clinical security.
Medical Disclaimer: This article is for general education and does not replace medical advice. Dialysis choice and schedules must be decided with your nephrologist based on your health, access type, and home support.
References
Yes, dialysis can be performed at home through Peritoneal Dialysis or Home Haemodialysis. Eligibility depends on medical stability, home hygiene standards, and caregiver availability. A nephrologist must assess suitability and provide structured training before initiation.
Home dialysis costs vary by modality and city. Peritoneal Dialysis involves recurring consumable expenses, while Home Haemodialysis requires significant initial equipment investment. Government schemes and insurance coverage can substantially reduce out-of-pocket expenses.
Adequacy testing is usually conducted every 1 to 3 months. It ensures waste removal meets clinical targets. Adjustments follow the nephrologist’s review.
Haemoglobin, potassium, phosphate, albumin, and creatinine require regular checks. Monitoring prevents complications like anaemia and electrolyte imbalance. Frequency depends on clinical stability.
Yes, uninterrupted power is essential for safe machine function. Backup power solutions are strongly recommended. Discuss contingency planning with your dialysis team.